

Life-Long Health Care
Close to Home
Life-Long Health Care
Close to Home
Washington Township Medical Foundation
Located in Northern California, we are dedicated to being the premier multi-specialty medical provider in the communities that we serve. Putting the patient first, we provide excellence in medical care and excellence in service through compassion, innovation and a focus on wellness, education and research.
Dedicated to being the Premier “Community-based” Medical Provider
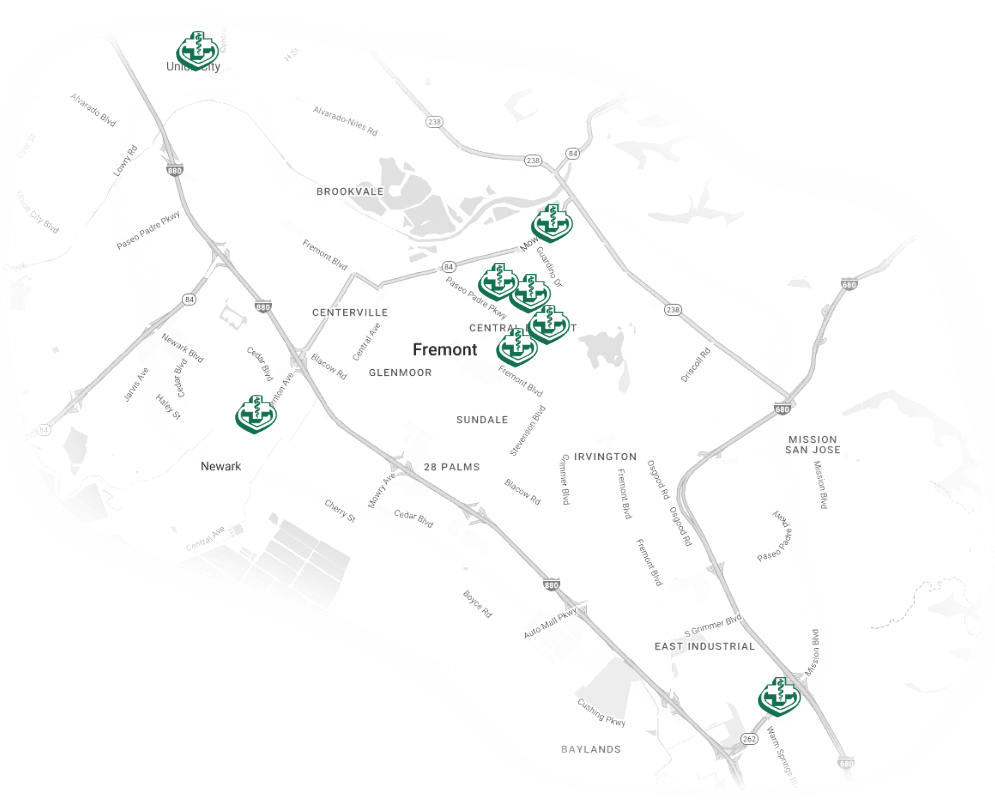
Our Locations
Washington Township Medical Foundation is set apart by our comprehensive areas of care. We are equipped to care for patients dealing with a variety of medical issues covering a broad range of services and specialties in the San Francisco Bay area.
View All Locations

Connect with Us
Upcoming Events
View a list of upcoming health education events for the community.
View All Events




